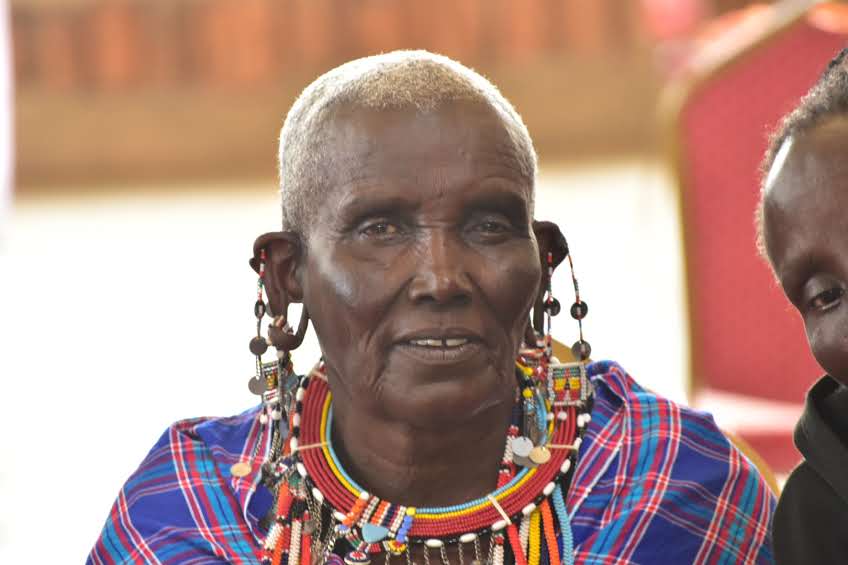
In Kenya, one in five maternal deaths is preventable—with timely care and community-informed interventions. From 10th to 12th December 2024, WEMA Health Foundation held an impactful Consultative Meeting for at least 107 TBCs in Imbirikani and 12 representatives from the county government, Kajiado County. This was not just another meeting—it marked a transformative moment in maternal health advocacy. Community Health professionals and TBCs came together to rewrite the story of maternal and newborn health in Imbirikani through engaging and insightful sessions facilitated by Dr. Elizabeth Makous, MSPT, Physical therapist and founder of Pelvic Whisperer, USA and Leah Wandera, Chief Executive Officer, WEMA.
The primary goal was to establish a collaborative framework between contemporary health stakeholders and traditional birth attendants to improve maternal and child healthcare in Kenya. Key objectives included:
- Educating participants on best practices in maternal and child health, integrating cultural considerations.
- Developing a community-based action plan to reduce maternal and neonatal mortality
Understanding Cultural Practices Around Birth
A group discussion was conducted to understand the traditional practices TBCs use when handling maternal health complications. TBCs and health providers engaged in a Q&A session, discussing their responses to various complications:
| Type of Complication | Response by TBCs |
| Severe Pain | Accompanying the mother and referring her to a hospital |
| Excessive bleeding | Administering herbal remedies, warm water, and transferring the mother to a hospital |
| Placenta retention | Inducing vomiting using beads or making the mother blow into an empty soda bottle |
| Nuchal cord (umbilical cord wrapped around the baby’s neck) | Using a single finger to return the baby to the uterus and untangling the cord via stomach massage with oil |
| Dizziness | Administering blood and milk |
| Fainted baby | Placing the baby in cold water or lightly pressing the hand vein to induce crying |
| Other | Praying for women who experience stillbirths |
Other challenges experienced by pregnant women discussed during this session included excessive bleeding d, obstructed and prolonged labor, and complications arising from twin deliveries that often require oxygen support. Participants also noted abnormal fetal positioning, frequent miscarriages, and rising cases of infertility within the community. Additionally, long distances to health facilities and low economic status were identified as major barriers that hinder access to timely and adequate healthcare for mothers and children.
Maternal Mortality and Neonatal Complications
During this session, Dr. Makous provided practical training on how TBCs can integrate medical knowledge with traditional practices to improve maternal outcomes. She demonstrated techniques for managing excessive bleeding, such as ensuring women lie down propped with a pillow rather than sitting upright. She emphasized the importance of involving men in childbirth and showcased supportive birth positions. Also, she highlighted the role of postpartum sex in promoting recovery and health and encouraged nipple stimulation during labor as a method to prepare for breastfeeding. Relaxation techniques, including singing and dancing, were recommended to help ease labor pains.
Furthermore, she educated TBAs on complications related to Female Genital Mutilation (FGM), introducing self-massage techniques to alleviate scar-related pain.
“As one gets old, the FGM scar gets hard, and FGM survivors should learn how to treat their own scars by pulling the tight parts. Releasing the scar releases the whole pain in the body to the back. They can do this through self-massage of the scar at the bottom of the vagina,” Dr. Makous explained.
To improve maternal and child health outcomes, several key recommendations were made during the consultative meeting. These included strengthening referral systems to support hospital deliveries and encouraging more frequent antenatal care (ANC) visits among expectant mothers. Capacity-building programs for Traditional Birth Attendants (TBAs) were emphasized as a means to enhance their skills and knowledge. The participants also highlighted the importance of fostering stronger collaboration between TBAs and healthcare providers. Additionally, the establishment of a reliable transport system for emergency cases was proposed, alongside the provision of contact information for nearby health facilities to ensure timely access to professional medical care.
Training, Data Sharing, and Action Plan Development
Health records personnel presented maternal and child health trends for the sub-county, highlighting key challenges: delayed ANC visits, low uptake of the 4th and 8th ANC visits, a rise in home deliveries, and increasing teenage pregnancies. While perinatal and maternal deaths have slightly decreased over the past three years, the rates remain concerning.
Several barriers to accessing quality healthcare were identified during the meeting. Poor healthcare services have discouraged many women from choosing hospital deliveries, while young primiparas (first-time mothers) often refuse hospital referrals altogether. Traditional Birth Attendants (TBAs) face challenges such as a lack of personal protective equipment (PPEs), largely due to policies that discourage home births. In the absence of proper birth plans, TBAs are often forced to use their own clothing during deliveries. Additionally, late referrals for teenage pregnancies were attributed to a general lack of public health education within the community.
Community Action Plan Development
During the community action plan development session, participants engaged in group discussions to identify key challenges affecting maternal and neonatal health (MNH) in Imbirikani. Among the major issues raised were knowledge gaps in managing MNH complications, delays in seeking hospital care, and widespread fear of cesarean section deliveries.
Some TBCs also reported a lack of recognition for their contributions, limited access to delivery kits—often forcing them to use nylon paper as gloves—and significant transportation difficulties, especially during adverse weather conditions.
“You might be called to go and assist a mother yet it’s raining and it’s far,” shared Mwende, a TBA, underscoring the logistical challenges faced in remote areas.
To address these concerns, participants proposed a series of actionable solutions. These included:
- Sensitization of TBCs through modern training.
- Strengthening referral systems for seamless coordination between TBAs and hospitals.
- Formal recognition of TBCs within the health system.
- Providing incentives for TBCs who escort pregnant mothers to hospitals.
- Improving services at healthcare facilities to encourage institutional deliveries.
- Increasing awareness on pregnancy danger signs through frequent community education.
- Supporting TBCs with PPEs such as gloves and cord clamps.
- Establishing an emergency delivery package to improve safety at home deliveries.
- Issuing identification tags for TBCs to formalize their role.
- Allowing TBCs to accompany pregnant women to ANC units for continuity of care.
- Facilitating transportation for emergency cases, especially in remote areas.
The consultative meeting marked a significant step toward improving maternal and child health in Imbirikani by fostering open dialogue between TBCs and healthcare providers. It provided a critical platform to address cultural practices, identify pressing challenges, and co-create practical, community-driven solutions. The discussions underscored the urgent need to strengthen collaboration, enhance training, and build support systems that recognize the vital role TBCs play in maternal healthcare.
Key recommendations emerging from the meeting include establishing a formal collaborative framework between TBCs and health providers, transitioning TBCs into trained professionals offering referral incentives to promote hospital deliveries. Equally important is improving access to delivery kits and personal protective equipment (PPEs), scaling up community education on antenatal care, and facilitating emergency transportation for laboring mothers. Collectively, these actions will help bridge the gap between traditional practices and modern healthcare, ensuring safer deliveries and better health outcomes for mothers and newborns in the region.